I think most people are familiar with the term cancer, as it is one of the world’s most common diseases. Growing up cancer was a common cause of death amongst me and my family and thus came familiar with the term. I can remember visiting my mother’s aunt who had cancer and witnessed and observed the drastic effects it had on her. This led me to believe that cancer was some sort of malfunction in the cells in our body and that it has the potential to spread to other areas of the body. In this blog I will share my knowledge and understanding of how cancer is such a simple concept on molecular bases and yet there is a high complexity in individual cancers making them difficult to treat. I will also briefly explain some similarities between the pathogenesis of cancer and auto-immunity.
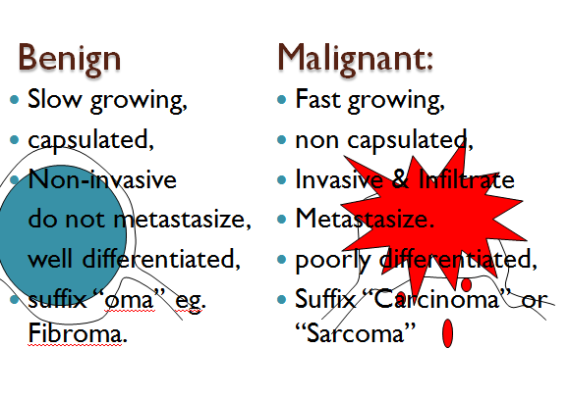
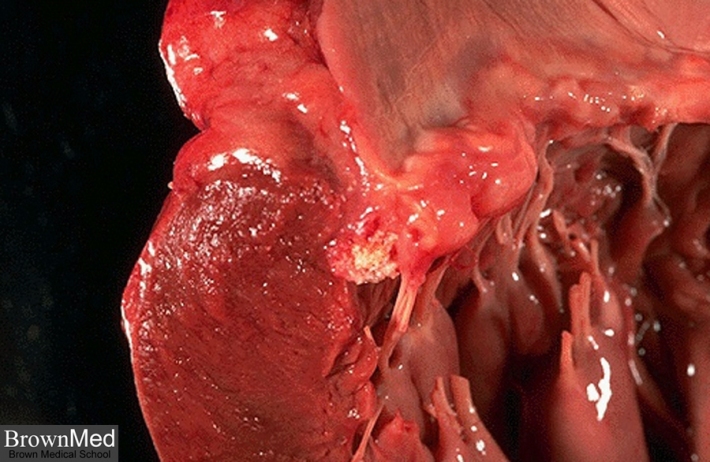
My perception of cancer was correct to some extent as cancer is caused by a tumor and tumors are masses of tissue or lumps caused by damaged cells that divide uncontrollably (MNT,2013). There are two types of tumors, benign and malignant tumors. A benign tumor is a growth that is not cancerous. This means it is localized and has not spread to other parts of the body or invaded and destroyed nearby tissue. In general, a benign tumor or condition is usually not harmful and benign tumors usually grow slowly. They can usually be removed and in most cases they never come back. However, if a benign tumor is big enough, the size and weight can press on nearby organs, blood vessels, and nerves and thus cause problems. The opposite of benign is malignant tumor. Malignant tumors are cancer, where the cancer cells can invade and damage tissues and organs near the tumor. Also, cancer cells can break away from a malignant tumor and enter the lymphatic system or the bloodstream (metastasise). This is how cancer spreads from the original tumor to form new tumors in other parts of the body (metastasise). Below is a picture showing the differences between benign and malignant tumors.
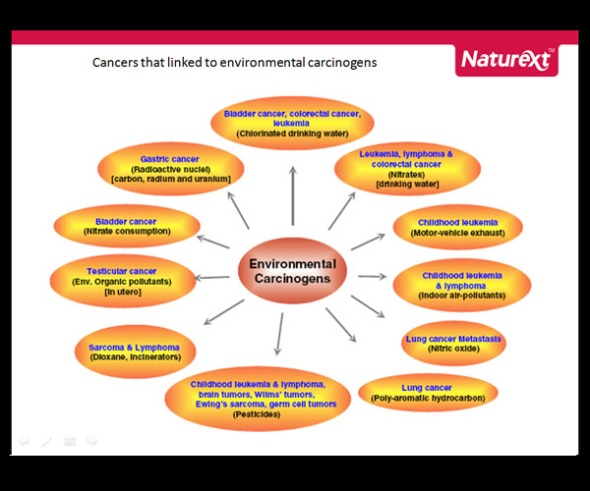
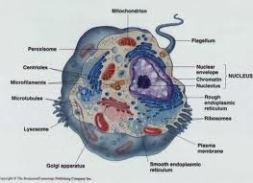
Each individual cancer is caused by a combination of things, some of which we can influence, such as lifestyle choices like smoking, and others that we cannot control, such as age and our genetics. Carcinogens which are cancer causing substances may damage cells and cause them to become cancerous due to gradual changes resulting from damage done to several of hundreds of genes that control cell growth, division and life span. If cancer were to be formed as a result of any of the above factors, the rate of growth may be slow if cancer is benign and rapid if malignant. Below is a picture that describes cancers thats linked to environmental carcinogens.
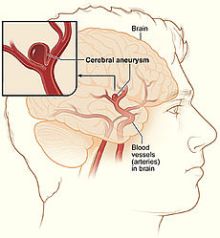
When we look at cancer defined as the abnormal cell growth of a damaged cell its referred to as a relative easy concept to grasp but when we observe the clinical, cytological, and histological differences of its manifestation it becomes highly complex and therefore difficult to treat. Let I remind you that cancer is not a disease where a microorganism is identified and then a treatment method is found. Cancer is an overgrowth of the body’s own cells which make identification and treatment much more difficult. Let’s take breast cancer for example. Breast cancer is a local spread and takes place by direct invasion and infiltration between tissues (Rippey, 2012). The tumor attaches to the skin and underlying fascia or muscle of the breast. As a result of such attachment the treatment is very complicated. A mastectomy must be performed and thereafter radiation is often recommended (Treating breast cancer, 2013). In addition malignant cells adhere less strongly to adjacent cells and thus have a tendency to metastasise by themselves (Rippey, 2012). Another good example is when tumors in the epithelial tissue invade the lymphatic system. When tumors are found in the lymph system local treatments become irrelevant and alternate treatments such as chemotherapy and the removal of the lymph come into play. The removal of the lymph would mean that the body would be left without any means to drain excess fluid in that particular area and could lead to lymph associated diseases such as lymphodema. Thus, treatment becomes very complex.Below is a video that shows how malignant tumors can spread to different areas of body.
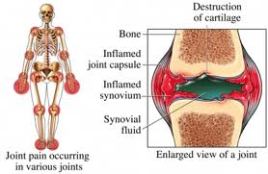
If you have an autoimmune disease, your own immune system attacks your body tissues. Normally, our immune system protects our body against infections caused by bacteria, viruses and other parasites. But if you have an autoimmune disease, your immune cells start to attack your own normal body cells. Therefore I would say that cancer and autoimmune diseases are similar in that they both cause normal cells to malfunction and as a result cause disease in the body. Another similarity between the two is shown when cancer develops in people who have particular autoimmune diseases. For example, people who have coeliac disease have a higher risk of non Hodgkin’s lymphoma and men who have a treatment called PUVA for psoriasis can have a higher risk of penile cancer (Cancer Research UK, 2012).
In conclusion, after reading through these modules my knowledge and understanding of cancer and autoimmunity has deepened and my perception on it has changed immensely. It is now clear to me that cancer is caused by malignant tumors and that cancers are highly complex and difficult to treat. As a result, I have great respect for patients that undergo treatments and bare the physical struggles of cancer.
References
Rippey, F F. (2012) ‘General Pathology’, Johannesburg, Witwatersrand University Press.
Martini and Nath. (2009) ‘Anatomy & Physiology’, San Francisco, Pearson Education.
Breast cancer. 2013 ‘Treatment of invasive breast cancer’ [online] Available at http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-treating-by-stage [Accessed 22 April 2013]
Cancer Research UK. 2013 ’Autoimmune diseases and Cancer’ [Online] Available at: http://www.cancerresearchuk.org/cancer-help/about-cancer/cancer-questions/autoimmune-disease-and-canc [Accessed 22 April 2013]
News Medical, 2013. What is cancer. [online] Available at: www.news-medical.net/health/What-is-cancer.aspx [Accessed 22 April 2013]